Introduction:
As of August 10, 2020, there have been over 5 million cases of the 2019 novel coronavirus disease (COVID-19) in the United States, resulting in 162,000 deaths. New York City became the first epicenter, with several case series based on over 56,000 hospitalizations and 18,900 deaths. These case series expanded our understanding of a broader clinical spectrum of COVID-19, extending beyond the initial descriptions of a viral pneumonia. This clinical spectrum has included arterial and venous thrombotic events. Factors upon admission, which are associated with development of thrombosis in hospitalized COVID-19 patients is less well defined. Our aim is to characterize the incidence of thrombosis and the associated clinical and demographic risk factors of patients hospitalized across a New York City hospital system.
Methods:
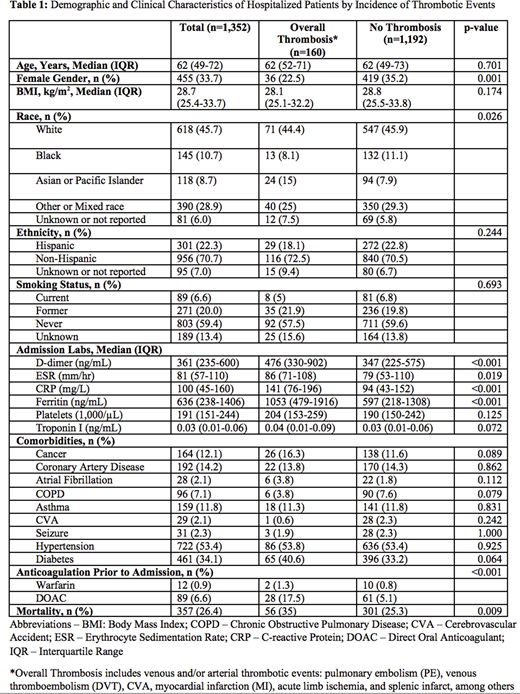
We conducted a retrospective observational study of all patients, age 18 and older, hospitalized with a reverse transcriptase-polymerase chain reaction (RT-PCR) confirming severe acute respiratory syndrome coronavirus 2 (SARS-CoV-2) infection between March 13 and April 4, 2020 in two hospitals in New York City. Clinical demographics, admission labs and medications prior to admission were collected. Thrombotic events were identified manually by chart review and were defined as experiencing arterial and/or venous thrombotic events, including pulmonary embolism (PE), deep vein thrombosis (DVT), cerebrovascular accident (CVA), myocardial infarction (MI), acute limb ischemia, and splenic infarct, among others.
Results:
There were 1,352 patients hospitalized during the study period. Overall median age was 62 years (IQR: 49-72), with 455 females (33.7%). There were 160 (11.8%) thrombotic events, including 102 with venous thromboembolism (VTE), 45 with PE, 69 with DVT, 32 with CVA and 55 with other thrombotic events (e.g. MI, acute limb ischemia, and splenic infarct). Females were 46% less likely than males to experience a thrombotic event (OR: 0.54 [CI: 0.36-0.79]). Patients who racially self-identify as Asian or Pacific Islander were observed to have a 2.06 odds compared to other races of having a thrombotic event with COVID-19 (95%[CI: 1.27-3.34]). Age, admission BMI, ethnicity, smoking status, and comorbidities were not associated with the incidence of thrombosis during hospitalization. Thrombotic events were associated with higher mortality in hospitalized COVID-19 patients (35% vs 25.3%, p = 0.009).
Conclusion:
Traditional risk factors (age, obesity, ethnicity, smoking status, and comorbidities) were not associated with an increased risk for thrombotic events in COVID-19 patients, while admission laboratory values (d-dimer, ESR, CRP, and ferritin) among patients experiencing an event were significantly different, highlighting the impact of the cytokine storm in mediating thrombotic events. Since the incidence of thrombosis associated with COVID-19 infection may vary according to clinical demographics, further investigation to identify high risk patients may enable us to consider the role of adjunctive treatment, such as therapeutic coagulation.
No relevant conflicts of interest to declare.
Author notes
Asterisk with author names denotes non-ASH members.

This feature is available to Subscribers Only
Sign In or Create an Account Close Modal